Requiring Daily Skilled Nursing Care
Your doctor must certify that you require daily skilled nursing care or skilled rehabilitative services. This care can include rehabilitative services by professional therapists, such as physical, occupational, or speech therapists, or skilled nursing treatment that require a trained professional, such as giving injections, changing dressings, monitoring vital signs, or administering medicines or treatments. This daily care must be related to the condition for which you were hospitalized.
If you are in a nursing facility only because you are unable to feed, clothe, bathe, or move yourself, even though these restrictions are the result of your medical condition, you are not eligible for Medicare Part A coverage. This is because you do not require skilled nursing care as defined by Medicare rules. However, if you require occasional part-time nursing care, you may be eligible for home health care coverage. For more information, see our article on Medicare’s home health coverage.
How Many Days Will Medicare Pay For Nursing Home Care At A Skilled Nursing Facility
Medicare Part A partially covers costs at an SNF for the first 100 days of each benefit period. A benefit period begins on the day that youre admitted as an inpatient to the SNF or hospital. It ends when you havent received any inpatient care at an SNF or hospital for 60 consecutive days. The Medicare Part A deductible restarts at the beginning of each benefit period.
The Medicare nursing home benefit variesdepending on the amount of time that youve been admitted.
- Days 1-20 you pay nothing
- Days 21-100 you have a daily coinsurance amount of $176 for each benefit period
- Days 101 onwards, youre responsible for all costs
Keep in mind that you need to ensure that the SNF accepts Medicare in order for Medicare to cover any costs. You can find an SNF thats certified by Medicare using their online tool. In addition, not all services may be covered at an SNF. For instance, Medicare wont cover a private nurse unless its deemed medically necessary. You can discuss your treatment with your healthcare provider to help ensure that the services they recommend are covered.
Whats A Qualifying Hospital Stay
Another important rule: You must have had a qualifying hospital stay, meaning you were formally admitted as an inpatient to the hospital for at least three consecutive days. You cannot have been in observation status.
In both cases you are lying in a hospital bed, eating hospital food and being attended to by hospital doctors and nurses. But time spent under observation does not count toward the three-day requirement for Medicare coverage in a skilled nursing facility.
When you enter the hospital, ask if you are being officially admitted or for observation. If the latter, you may want to appeal to your doctor to see if you can be switched to inpatient status. Two more things to note about the three-day rule:
- Medicare Advantage plans, which match the coverage of original Medicare and often provide additional benefits, often dont have those same restrictions for enrollees. Check with your plan provider on terms for skilled nursing care.
- Skilled nursing facilities are the only places that have to abide by the rule. If youre discharged from the hospital to another kind of facility for ongoing care, such as a rehabilitation hospital, Medicare provides coverage under different rules.
If you qualify for short-term coverage in a skilled nursing facility, Medicare pays 100 percent of the cost meals, nursing care, room, etc. for the first 20 days. For days 21 through 100, you bear the cost of a daily copay, which was $170.50 in 2019.
You May Like: How Do I Apply For Medicare In Missouri
Federal Requirements Specify That Each Nf Must Provide At Least:
- Nursing and related services
- Specialized rehabilitative services
- Medically-related social services
- Pharmaceutical services
- Dietary services individualized to the needs of each resident
- Professionally directed program of activities to meet the interests and needs for well being of each resident
- Emergency dental services
- Room and bed maintenance services
- Routine personal hygiene items and services
Original Medicare And Nursing Home Benefits

In Your Guide to Choosing a Nursing Home or Other Long-Term Services & Supports, the Centers for Medicare & Medicaid Services says that if you have Original Medicare, a majority of your nursing home care expenses will not be covered.
While there are some benefits under Part A , they are extremely limited and typically only apply to medically necessary skilled nursing care due to an illness or injury that meet specific conditions. Even then, theyre generally only covered for a limited time.
Medicare does offer at least partial benefits toward the following, among others, according to Medicare.gov:
- Skilled nursing care
- Medical supplies used while in the facility
- Ambulance transportation
- A semi-private room
- Meals and dietary counseling
To be eligible for coverage related to these skilled nursing care expenses, participants must have a qualifying hospital stay , have days left in their benefit period, and choose a facility that works with the Medicare program.
The skilled nursing facility must also be doctor-recommended, and will generally only be covered for patients with a hospital-related medical condition or a condition that started while already in a skilled nursing facility.
Medicare-approved health insurance plan, the CMS says that the individual plan dictates whether any nursing home care coverage is provided and, if so, to what extent.
Read Also: How To Change Medicare Direct Deposit
Medicare Coverage Of Home Health Care
Another option for seniors who need assistance is home health care. When this service is ordered by a doctor in place of in-patient treatment, its covered by Medicare. Speech, occupational and physical therapy can often be provided at home instead of in a care facility. Home health care coverage is usually temporary, but it may become long-term for seniors as an alternative to full-time care in a nursing home.
Long-term care insurance can fill the gap in paying for both nursing home care and home health care. Insurers may cover only certain types of nursing home facilities and home health care providers, and some policies exclude pre-existing conditions. Thats why its vital to do your homework and choose wisely among providers licensed by the state where you live.
What Is Skilled Nursing Care
Skilled nursing facilities are sometimes called post-acute rehabilitation centers, but the rules for a stay in an acute care rehabilitation center, or inpatient rehab facility , are different. For more information, see our article on Medicare coverage of inpatient rehab facility stays.
Skilled nursing facility care, which takes place in a hospital’s extended care wing or in a separate nursing facility, provides high levels of medical and nursing care, 24-hour monitoring, and intensive rehabilitation. It is intended to follow acute hospital care due to serious illness, injury, or surgeryand usually lasts only a matter of days or weeks.
In contrast, most nursing homes provide what is called custodial careprimarily personal, nonmedical care for people who are no longer able to fully care for themselves. Custodial care often lasts months or years, and is not covered at all by Medicare. For the most part, custodial care amounts to assistance with the tasks of daily life: eating, dressing, bathing, moving around, and some recreation. It usually involves some health-related matters: monitoring and assisting with medication and providing some exercise or physical therapy. But it is ordinarily provided mostly by personnel who are not highly trained health professionals and does not involve any significant treatment for illness or physical condition.
Don’t Miss: What Is The Best Medicare Supplement Insurance Plan
Who May Receive Nursing Facility Services
NF services for are required to be provided by state Medicaid programs for individuals age 21 or older who need them. States may not limit access to the service, or make it subject to waiting lists, as they may for home and community based services. Therefore, in some cases NF services may be more immediately available than other long-term care options. NF residents and their families should investigate other long-term care options in order to transition back to the community as quickly as possible.
Need for nursing facility services is defined by states, all of whom have established NF level of care criteria. State level of care requirements must provide access to individuals who meet the coverage criteria defined in federal law and regulation. Individuals with serious mental illness or intellectual disability must also be evaluated by the state’s Preadmission Screening and Resident Review program to determine if NF admission is needed and appropriate.
Nursing facility services for individuals under age 21 is a separate Medicaid service, optional for states to provide. However, all states provide the service, and in practice there is no distinction between the services.
In some states individuals applying for NF residence may be eligible for Medicaid under higher eligibility limits used for residents of an institution. See your state Medicaid agency for more information.
Are Nursing Homes Covered By Medicare And Medicaid
Few domestic issues are more controversial than the national healthcare system, and with good reason: recent studies have shown that medical bills are the number one cause of consumer debt and bankruptcy in the United States. With healthcare costs continually rising, many seniors worry about how they will pay for for their nursing home stays. Fortunately, theres good news: many nursing homes accept Medicaid and Medicare coverage. In this blog post, Philadelphia nursing home abuse attorney Brent Wieand will explain elderly citizens legal rights when it comes to receiving care at Medicaid- and Medicare-certified nursing homes.
Don’t Miss: What Is A Medicare Special Needs Plan
What Kind Of Care Do Nursing Homes Provide
Nursing homes give care in both of these general areas:
- Custodial care is help with daily activities such as dressing, eating, and bathing.
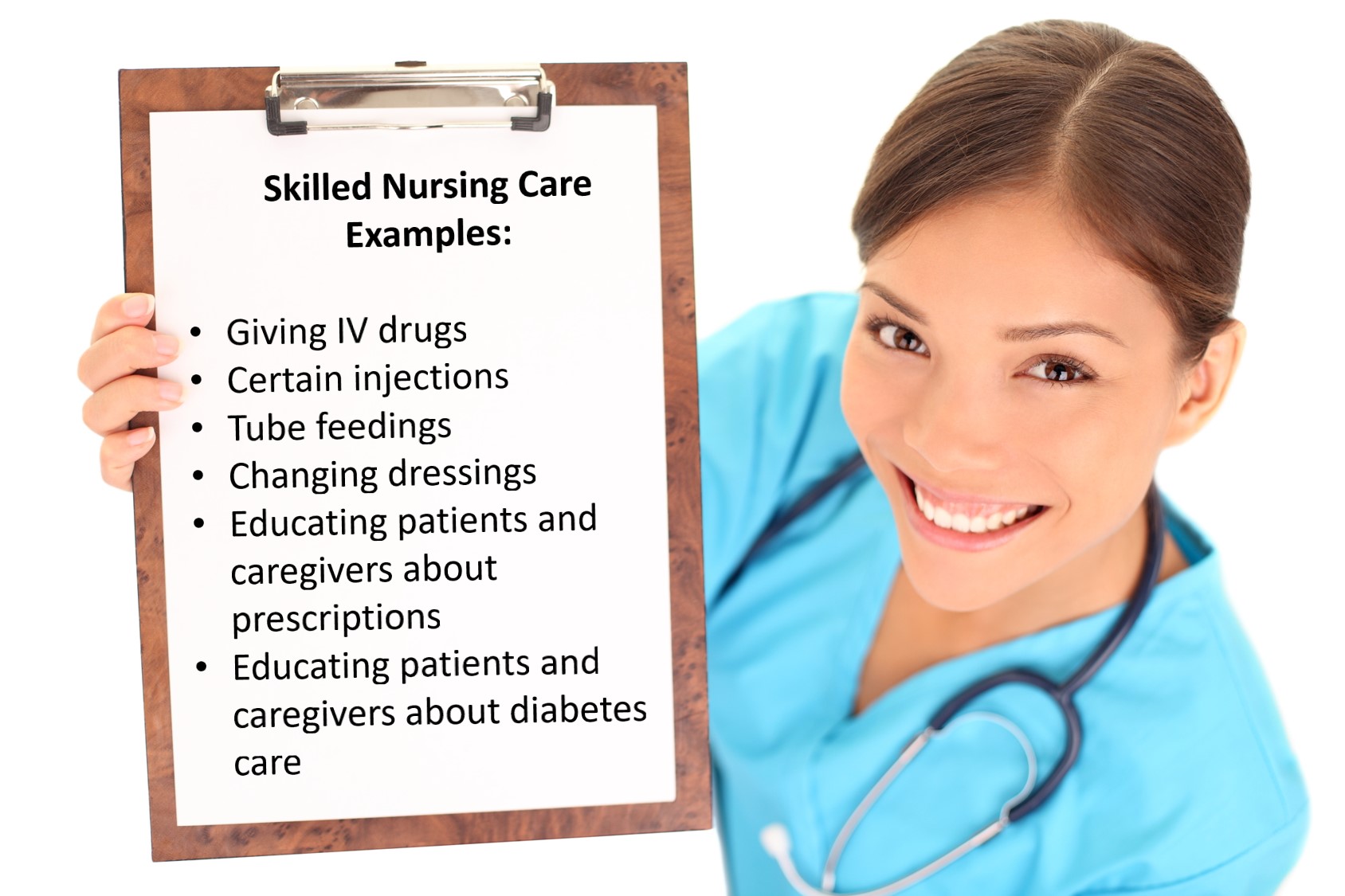
- Skilled nursing care is given by a nurse or rehabilitation specialist to manage, observe, and evaluate your care. It can include medication management, wound care, dialysis, and more .
Nursing homes are not just for eldercare. They can also provide:
- Rehabilitation services the goal of this kind of care is to help your condition improve so that you can eventually live on your own. For example, if you have major surgery and are released from the hospital, your doctor might order rehabilitation services for you until you recover enough to live independently at home.
- Long-term care for a serious illness, such as multiple sclerosis .
What Is A Nursing Home
A nursing home is a place where a person can receive extra care services from nurses or nurses aides.
Many of these facilities may be homes or apartments for people who need extra care for their daily activities or who no longer desire to live alone. Some resemble hospitals or hotels with rooms with beds and baths and common spaces for classes, recreation, eating, and relaxing.
Most nursing homes provide around-the-clock care. Services can vary, but may include help to go to the bathroom, assistance getting medications, and meal services.
Recommended Reading: Does Medicare Cover International Medical Emergencies
How Much Does Medicare Pay For Nursing Home
Medicare pays for limited services in a nursing home. Original Medicare covers only medically necessary, skilled care at a long-term care facility.
However, most care that occurs at a nursing home has to do with daily living, like bathing, dressing and using the bathroom. These ânon-medically necessaryâ services would not be covered.
However, this only works at a Medicare- or Medicaid-certified long-term care facility.
When Does Medicare Pay For Treatment In A Nursing Home

Its sometimes easier to grasp what Medicare covers at a nursing home by first understanding what it doesnt cover. When a person merely needs custodial care, Medicare does not cover the cost of care in a nursing home. The following services are included in custodial care:
- Bathing
- Eating
- Using the toilet
In general, if a person needs care that does not require a degree to perform, Medicare will not pay for it.
Lets take a look at what Medicare does and does not cover.
Its also worth noting that this is only a short-term solution, not a long-term solution.
In most cases, Medicare Part A will cover up to 100 days of treatment in a skilled nursing facility. The person must be admitted to a skilled nursing facility within 30 days of leaving the hospital, and they must be admitted for the disease or injury for which they were getting hospital care.
Don’t Miss: Does Medicare Cover Prolia Injections
If You Require Nursing Home Care In The Coming Year Which Medicare Plans Should You Choose
The majority of Medicare plans do not cover nursing homes. If you enroll in a Medicare Advantage plan through a special arrangement with a nursing facility, you may be eligible for an exemption from the rule on enrollment. This is the exception rather than the rule, and the alternatives vary depending on the region.
Do Assisted Living & Memory Care Facilities Accept Medicare Or Medicaid
As healthcare costs continue to rise, you may wonder how your parents are going to cover the expenses. According to Genworth Financial, an average assisted living community costs $43,200 each year. Skilled nursing communities range between $80-and-$90,000 a year for semi-private and private rooms, respectively. Memory care facility costs are almost $69,000 annually, on average, according to data from the Retirement Living Information Center.
Its important for adult children and family caregivers to understand the expenses that relate to senior living communities. This includes discovering what is and isnt covered by Medicare and Medicaid.
Read Also: Will Medicare Pay For A Bed
Does Medicare Pay For Home Care Nursing
If you meet the requirements for home health care, Medicare generally covers part-time, intermittent home care nursing and other medical therapies, such as physical and occupational therapy. If the home care nursing follows a qualifying hospital stay, Part A may cover 100% of allowable charges.
If there was no qualifying inpatient hospital stay, Part B may still cover some home care nursing services.
Medicare typically doesnt pay for more than eight hours a day of home care nursing, and it typically doesnt cover services seven days a week. Medicare only covers home care nursing for a short period of time.
If you qualify for hospice care and choose hospice benefits under Part A, Medicare pays for part-time home care nursing for as long as you receive hospice care.
Your Nursing Home Costs In :
- Medicare generally pays 100% of the first 20 days of a covered nursing home stay.
- Days 21 to 100: $185.50 coinsurance per day of each benefit period. You pay coinsurance for each day of the benefit period.
- If you stay in a skilled nursing facility longer than 100 days per benefit period, Medicare typically stops paying nursing home costs.
Read Also: How Do Zero Premium Medicare Plans Work
What Does Medicare Advantage Cost
In most cases, Medicare beneficiaries with Original Medicare dont pay for Part A coverage but have a monthly premium for Part B coverage. In 2021, the standard Part B premium is $148.50. Seniors with Medicare Advantage plans are also required to pay this monthly premium and may also have an additional monthly premium for their specific plan. On average, Medicare Advantage premiums are $21 per month in 2021, and nearly half of enrollees have no additional premium.
What Is Medicare Part A
Medicare Part A is part of Original Medicare, along with Medicare Part B . Part A is usually premium-free.
It covers but is not limited to inpatient care in a hospital, skilled nursing facility care, short-term nursing home care, hospice care, and home health care. If youre in a Medicare Advantage Plan or other Medicare plan, that plan may have different rules. But your plan must give you at least the same coverage as Part A Original Medicare.
Also Check: Do I Qualify For Medicare If I Am Disabled
Finding The Right Nursing Home For You
To find and compare Medicare-certified nursing homes in your area, Medicare.gov offers an online search based on where you live.
The site also offers a Nursing Home Checklist to take with you when visiting potential homes in person. This document provides a number of factors to consider before deciding on one, such as:
- Staff actions and appearance
- The state of the living spaces
- Resident room space and rules
- Menu and dietary options
What Does Medicare Advantage Cover
Health insurance companies that offer Medicare Advantage plans are required to cover the same services and benefits that are included in Original Medicare, and they cannot charge a co-pay or coinsurance for services that are covered 100% under the standard Original Medicare policy. Some medical services that are covered include:
- Hospital care
- Adult day health care
You May Like: How Do I Check On My Medicare Part B Application
How Does Medicare Affect Long
Medicare is a government-managed health insurance program designed to assist people 65 or older in paying for certain healthcare costs.
That said, many people are surprised to learn that Medicare does not always cover every medical expense in every situation. For example, long-term nursing home care is not typically covered by Medicare benefits.
However, there are a few aspects of nursing home costs that may be covered under certain parts of Medicare. Learn more about Medicare and nursing home coverage right here at MedicareInsurance.com.
Home Health Care Benefits
Home health care provides a range of health care services in your home for an illness or injury. Services could include wound care, patient and caregiver education, intravenous or nutrition therapy, injections, or monitoring serious illness and unstable health.
Home health care can help you regain your independence, become as self-sufficient as possible, maintain your current condition or level of function, get better, or slow decline.
It is also usually less expensive, more convenient, and as effective as the care you receive in a hospital or Skilled Nursing Facility . Usually, a home health care agency coordinates the care your doctor orders for you.
Your home health care is Medicare-eligible when you:
- You have Medicare Part A.
- You are under the care of a doctor and are receiving services under a plan of care created and reviewed regularly by a doctor.
- Your doctor must certify that you need intermittent skilled nursing caresuch as blood drawn. Or physical therapy, speech-language pathology, or continued occupational therapy. Read the additional criteria for when youre eligible for these services and when Medicare covers them.
- The home health agency caring for you is Medicare-certified.
- A doctor certifies that you are homebound. This means that you cannot leave your home without substantial effort. Or it is medically unadvised that you leave home without the help of another person, transportation, or special equipment.
What Home Health Care is Covered?
You May Like: Does Medicare Cover Bladder Control Pads
